Archives for rehab (page 4)
May 9, 2004
Going bananas
 Every hour, every day
Every hour, every day
I hit the floor to combat decay.
On the floor I twist and extend
I am the banana, or so I pretend.
This piece of sub-standard poetry goes merely an inch of the way in conveying my happiness about being almost straight again. The protective cramp is not totally gone yet, but today my right shoulder is drooping just slightly. I saw some improvement already Saturday morning, but I regressed almost to square one after I dropped my credit card while shopping for eggs and some milk. In an effort to look half normal, I went down on one knee to pick it up with the result that not only my back tightened up, but also my abductor muscle on the left leg (at first I feared I had caused muscle damage, now I suspect it was merely a cramp). Took a while to limp home and do the banana extension again.
This morning I was nearly straight, but I had the worse pain yet quite evenly distributed over the lower back. Before it had been almost exclusively on the left side. This is actually a good sign according to the McKenzie method, named after its founder New Zeelander Robin McKenzie. The theory, known as the “dynamic internal disc model”, is that back pain is generally due to the fluid nucleus of the discs being displaced, causing them to put pressure on surrounding nerves or the disc annulus itself (article about how the discs work). Sometimes the pinched nerves cause pain to radiate down into the buttocks and/or legs, sometimes it is more local like in my case. By assessing which end range movement (bending as far as one can in one direction) lessen pain for the patient (usually bending backwards, i.e. extension) and having the patient do this exercise frequently throughout the day, the displaced fluid material should gradually return to normal. As the pressure on the nerves is gradually decreased, the pain will tend to move away from the periphery of the legs and buttock towards the center of the back after which it should disappear completely if the end range movement is continued. As McKenzie has made clear in one of his books that I borrowed from the library, Treat Your Own Back, that pain might actually increase during this process.
Now, pain does not centralize for all patients, in case of which there is a problem that should be dealt with by other means. The McKenzie method has actually shown to be effective both in separating patients with disc problems from patients with non-disc problems and in determining whether the disc annulus is intact or not.
The elicitation of pain “centralization,” an improvement (favorable change) in pain location in response to repetitive end-range testing, typically occurring with only one direction of test movement(s), predicts a high likelihood of successful response to conservative care, even in the presence of neurological deficits. Irreversible conditions are characterized by symptom aggravation by all directions of testing, including the absence of the centralization response, predicting a poor response to non-surgical care. In those whose pain is unaffected with similar testing, evidence indicates the pain is likely nondiscogenic. A dynamic disc model has been described as a possible model for these varying pain responses. Insight into annular integrity of symptomatic discs is also provided using this repeated end-range/pain response (McKenzie) assessment.
Wetzel FT, Donelson R. The role of repeated end-range/pain response assessment in the management of symptomatic lumbar discs. Spine J. 2003 Mar-Apr;3(2):146-54.
In fact, McKenzie has even been shown to be more effective than MRI (magnetic resonance imaging) in this regard, which might explain why my back therapist thought a MRI was not necessary at this stage.
The McKenzie assessment process reliably differentiated discogenic from nondiscogenic pain (P < 0.001) as well as competent from an incompetent anulus (P < 0.042) in symptomatic discs and was superior to magnetic resonance imaging in distinguishing painful from nonpainful discs.
Donelson R, Aprill C, Medcalf R, Grant W.: A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine. 1997 May 15;22(10):1115-22.
At this point in my treatment, the aim is to see how my back reacts, which should help provide some clues as to what the continued treatment should look like. I believe I probably have some soft tissue problem left from December, so even when pain is gone there will probably be some healing left to do. I am not yet a 100% sure that the pain is centralizing for good, but I do know that the banana extension helps ease pain tremendously.
If I am straight tomorrow, I might go ahead and do my ME Bench workout. If in any doubt, I will rest instead. It seems like the biggest changes in my posture takes place during the sleeping hours, at least thus far. It actually feels a little bit like Christmas to wake up and get in front of the mirror to see whether there has been any improvements. In the spirit of this, I bid you good night and good back health!
Further reading:
Louis Kuritzky and Jacqueline White: Extend Yourself for Low-Back Pain Relief. The Physician and Sportsmedicine, vol 25:1, January 1997.
May 6, 2004
McKenzie - the final solution?
Waking up this morning the cramp from yesterday had eased a little, but I still looked like one crooked bastard. Unlike yesterday, I was actually able to bend to the right a little. Needless to say, I did not go to work today. Instead I stayed home and felt grateful that I had an appointment with a back specialist in the afternoon.
I was met with a friendly greeting at the clinic, the kind of service uncommon outside the private healthcare sector. The waiting room was filled with pictures showing off acrobatic feats and healthy spines. I can see how some patients might become a little depressed by this after struggling to reach the clinic with an aching back, but I liked them for what I presume was the reasons they were put there in the first place. Help just around the corner. But then, I assessed my pain level as a modest 5 on a scale of one to ten on the registration form… With a major nerve impingement the trapeze dolls could have been in grave danger.
The therapist, a guy about my age, was inspiring and talkative. First we sat down and went through my injury and treatment history. I had actually prepared a somewhat detailed outline that I handed him. Thanks to this blog, it was a breeze to write down exact dates and details that otherwise would have been but foggy estimations.
Underwear time! He had me do repetitions of ten bending in different directions in order to assess whether a certain movement aggravated or lessened the protective response and pain. After I finished a movement his trained eye scanned me for minute changes in posture. He had me bend forward as far as I could go (painful), backwards (felt surprisingly good afterwards), to the left (so so) and to the right (not painful).
He told me that he was assessing me using the McKenzie method, which he proceeded to outline in some detail. If I understood him correctly, he explained that the fluid nucleus of the discs can be displaced causing overstretching of soft tissue around the vertebrae, which in turn would cause pain. The task of the assessment movements is to determine in which direction the spine has to be moved in order to counteract, and ultimately correct, the displaced fluid nucleus. After it was clear that extension (bending backwards with hands clapped around the lower back) caused relief, something that apparently is usually the case, he had me lie down on the table.
First he checked my mobility, such as seeing how far forward he could lift my legs before pain set in while I was lying on my back. Lifting the right leg it started hurting in the back first, with the left it was the hamstrings. After giving him an affirmative answer to the question of whether the osteopath had adjusted my spine, he also had me lie on both sides in turn and he pushed down hard on the leg bent on top. He didn’t do it with quite as violent leverage as the osteopath had, and I could not feel any cracking. I got the impression that he felt that it was way too early to do any heavy adjustments, but these quick jerks showed him that my back is elastic and responsive.
He then turned me on my stomach and had me do ten repetitions of pushing my upper body up with my arms as far as it would go (known as the cobra position in yoga). Then this was repeated in what he called a banana position, where the feet were pushed to the left and the hip to the right (hip away from the pain that is primarily to the left of the lower back). Indeed, I felt like any ripe banana in this position. It did not feel half bad.
Concluding a visit that had lasted a leisurely 40 minutes or so, he wanted to know whether I would be willing to come in for further sessions. Although my wallet is not as full as I’d like it to be, I naturally said yes. We booked a time for next week’s Tuesday, when another therapist will test me on various exercises in their rehab room. The idea here is that she will form her own opinion independent of his and then we will together think of a suitable approach to healing. “Scientific”, I remarked. It might be a McKenzie approach or something else; preliminary he told me that my case shows some deviation from the standard case.
In the meantime, he told me that I should do repetitions of ten in the banana position once every hour and any of the other movements we had tested that felt good. Self-assessment is key in this phase.
This visit left me feeling quite good. Although I confess to having hoped that he would crack me straight (in retrospect I can see why this would not make much sense at the moment, cf. Vince’s excellent comments) and felt a little tender from all the end range of motion movements, especially the forward bending that made me hurt at the spot of the original injury, I was very impressed his thoroughness and willingness to listen and discuss. He agreed with my thoughts on trigger points and was very encouraging when it came to my training. Before the visit I had visions in my head of him shaking his head when he heard that I injured myself doing a good morning (”stupid stupid”), but no. He also agreed that I could well continue my bench workouts as normal, although I might consider going a little lighter than singles. I mentioned doing reverse hypers and that they did not seem to aggravate my condition and he gave the green light for those as well. Not that I feel like doing any of those, or any benching for that matter, before my body is upright again.
This continuing back pain saga is inducing a split personality… On the one hand it sucks that I haven’t been able to go for any deadlift or squat records in five months, but on the other hand I am intensely intrigued by this opportunity to learn more about how my body works. I am now doing things with tennis balls and banana shapes that I could not have dreamed of before. I also hope that these posts might be of some help to others with similar injuries, while functioning as a gentle reminder to the healthy among you. Lift strict, learn what you can ahead of time and never hesitate to consult professionals. I for one will be very happy about this knowledge once I get old enough to walk around with a cane. Perhaps I won’t even need one.
May 5, 2004
Gordian knots
 Back to Westside for the squat/dead workouts as well. Preliminary, I am striving to at least do the max effort day while keeping the dynamic day as an option if my back is up to it. I think I might be able to box squat, which I find easier on the back than normal squatting. After my back completely locked itself up last time I did freeweight squatting in March, I figured I would play it safe and do Smith squat for a while before starting to work with Mikesell. Indeed, Smith squats served me well one month after I ripped my back.
Back to Westside for the squat/dead workouts as well. Preliminary, I am striving to at least do the max effort day while keeping the dynamic day as an option if my back is up to it. I think I might be able to box squat, which I find easier on the back than normal squatting. After my back completely locked itself up last time I did freeweight squatting in March, I figured I would play it safe and do Smith squat for a while before starting to work with Mikesell. Indeed, Smith squats served me well one month after I ripped my back.
Smith squat I did. But not for long. Felt some acute discomfort already at 60 kg/133 lbs. Taking what I perceived to be the rational path, I aborted the squatting and started hauling 10 kg/22 lbs plates up to the second floor for my makeshift reverse hypers. Could feel my gluteus and back tightening up at this point, so I dashed down to the locker room for my trusty tennis ball. After doing a quick perverse looking trigger point massage for the gluteus, I felt ready to begin. Went well. Before I knew it I had completed the workout that is by now becoming my fallback routine, the Happy Back Workout®, when I am hurting. Armed with a set of fully loaded batteries, my friend and occasional training partner Måns made my digital camera sing and filmed all exercises (VIDEO 3.2M).
Mixed up my protein shake and headed for the sauna. While drying myself I happened to catch a glimpse of my shoulders in the mirror, and noticed that my shoulder girdle appeared to be slanting to the right. The more my body cooled down, the more the pain in the lower back increased. Sitting on the bus, I decided that this was the last straw as I refuse to be hurting five months after my initial injury without a battle. As soon as I got home I booked an appointment to a private highly regarded back clinic, Selkäcenter, for tomorrow afternoon. By this time my body was already slanting heavily to the right indicative of what I think is a protective cramp caused by my body trying to protect the old injury, which I now believe is probably not quite healed. Challenges abound.
Smith machine squat:
6 @ 40 kg/88 lbs
3 @ 60 kg/133 lbs (back discomfort - aborted here)
Reverse-hyper, done off hyper bench with weights between legs:
30 @ bodyweight
15 @ 10 kg/22 lbs
15 @ 20 kg/44 lbs
15 @ 30 kg/66 lbs
15 @ 35 kg/77 lbs
Ball crunch:
20 @ bodyweight
10 @ 5 kg/11 lbs
10 @ 10 kg/22 lbs
10 @ 12.5 kg/28 lbs
10 @ 15 kg/33 lbs
30 @ bodyweight
Seated calf raise:
worked up to 8 @ 90 kg/199 lbs
Total training time: about 90 min, which included trigger point massage etc.
April 8, 2004
Osteopath revisited
Two weeks have elapsed since I had my spine mobilized by the osteopath. Although it did not remove the pain altogether, my back has started feeling quite good during the last few days. Sitting on the metro for my second appointment, I was, ironically enough, hoping that this visit would not destroy the status quo by upsetting my temperamental spine hound too much.
After again stripping down to my bare essentials, he had me bend left and then right. Left I could go really far, but I had considerably less mobility bending to the right. No pain, I was just feeling stiff in that direction. After stating the obvious, the therapist had me lay down on my sides and cracked my lower back in the same fashion as last time. This time it went easy and the pops were not as major. The upper back was another story. Lying on the back with his fists between me and the bench, I could both feel and hear a major part of my upper spine jumping into place over several vertebrae. All I could say was something akin to “holy camolie!!”. Six on the Richter scale.
Lying on my back with hands clasped behind my neck, he then cracked my upper back/neck by turning my upper body sideways. Nothing major, but quite enjoyable nonetheless. Massaging my gluteus, he concluded that my left one was considerably less tight than last time, but the right one was still somewhat stiff. My hamstrings were really tight, part of which is probably due to the reverse-hypers I did three days ago.
He approved of the tennis ball massage I have been doing several times daily, and said that I could do it for the hamstrings too. “Put two balls in a sock, and you will get a very effective massage tool”. Concluding the treatment, he said that things were starting to look quite good. Although my upper back had jumped out of alignment between treatments, the natural curvature of the upper spine had returned making it much less flat. The lower back was also in much better shape, and the gluteus trigger points much weaker. “I don’t think you need to come back, but if you feel you need it, you know where to find me. Close the door when you’re done dressing”.
April 5, 2004
Happy back workout
This was a good one. Skipped all fancy footwork and simply pyramided up on reverse-hypers, ball crunches and seated calf raises. Haven’t done reverse-hypers in a while, probably because I was pushing the limit on how much weight my dress belt could handle. Found a short piece of wire at the gym, which I used together with two ankle belts to wrap plates around my ankles. The only problem with this was that I twice managed to wrap them so thoroughly that it took me several minutes to unknot… Worked up to 30 kg/66 lbs doing them off a normal hyperextension/back raise, of course mounting it the “wrong” way (hands grabbing the feet support). Next week I might take a clip of these.
A really nice and back-friendly workout. Currently, reverse-hypers (even if not done on the real thing that allows the disks to open up at the bottom) and pull-throughs are my best recommendations for exercises to do when the back is not quite up to par. What they have in common is that both are heaviest at the top of the movement (legs in line with upper body). Compare this to good mornings, where the heaviest part is at the bottom (bent forward at the waist) where the lower back is at its most vulnerable. Both type of exercises have their place (force curves should be varied for optimal strength and stability), but when it comes to rehab I think it is wise to concentrate on those which are heaviest at the top, not the bottom. Just my 2 cents.
Reverse-hyper, done off hyper bench with weights between legs:
30 @ bodyweight
15 @ 10 kg/22 lbs
15 @ 15 kg/33 lbs
15 @ 20 kg/44 lbs
15 @ 25 kg/55 lbs
15 @ 30 kg/66 lbs
30 @ bodyweight
Ball crunch:
30 @ bodyweight
10 @ 5 kg/11 lbs
10 @ 10 kg/22 lbs
8 @ 12.5 kg/28 lbs
20 @ bodyweight
Seated calf raise:
10 @ 40 kg/88 lbs
10 @ 55 kg/122 lbs
10 @ 70 kg/155 lbs
8 @ 80 kg/177 lbs
Total training time: 65 min
March 31, 2004
Some highly-valued feedback
Yesterday I got a back pain companion in Vincent Scelfo, who e-mailed me with the unfortunate news that he too had sustained a soft tissue injury doing good mornings. Vince is an old hand in powerlifting, having back in 1978 set New Jersey state records in the 123 pound/56 kg class, with a 440 lbs/199 kg squat, a 445 lbs/201 kg deadlift and a 1085 lbs/491 kg total. Of course, these lifts were achieved without the dubious benefits of today’s highly developed equipment. After a long layoff, he is now back re-building his strength using Westside methods.
Vince is in quite good hands with his unfortunate injury, i.e. his own, as it turns out he is a practicing chiropractic. He graciously agreed to let me post an excerpt from our correspondence, which I think adds some much needed perspective on my recent entry on trigger points.
I have been a chiropractor for over 22 years. Over the years I continually formulated my own thoughts and opinions, some of which may be totally opposite of what is taught to the general chiriopractor. This is one reason
why I became an upper cervical specialist.I have read the accounts of your injuries and I would say that you are fairly close to what I believe.
From a philosophical viewpoint, chiropractic talks about the subluxation (misaligned vertebra that produces pressure on a nerve). The result of which can be pain or illness. I do hold to this basic premise of our profession.
Where I have a problem is when things occur like a back injury. You lift something that’s too heavy. You injure the soft tissue (muscles, ligaments, joints, discs). Inflammation occurs in the tissue and you get PAIN!
The chiropractor says, “Here’s your problem, you have a bone out of place.” He adjusts you and you get some relief. The wonders of chiropractic! But now you have to keep going back 20 or 30 times to “fix” it.
The question I began asking myself was, did the bone out of place cause the
problem or was the muscle injury the reason the bone is now out of place?
There is a tremendous difference.This is where I began changing my thought about the whole mechanism of injury in relation to the chiropractic principle. It only makes sense (at least to me) that if you injure the muscle, when the muscle becomes spastic the bone is going to move and be out of position. Unfortunately, these problems are seen as “bone” problems and not soft tissue injuries which require healing.
This is why I don’t work on low backs. Instead, if you can balance the framework which is controlled by the nerve centers in the upper spinal cord, that will balance the structure. This allows the muscles to come back to normal tone and heal. I don’t have to keep “racking” a bone in place day in and day out. In the injury situation, the bone out of place is the EFFECT, not the cause. It has shifted because of injury to the soft tissue or joint. When the soft tissue heals, the bone will go back to its normal position.
This is where, in my opinion, chiropractors make a grave mistake. They adjust the bone. But it never stays in place. So you keep going back over and over.
Get the system balanced and give it time to heal.
Disc problems require long time to heal. Symptoms can be extremely painful. Joints also. Ligaments are not elastic and when injured may not return to full strength as they heal up with scar tissue. Muscle strains heal up pretty readily.But the body does heal. Some things quicker than others and depending on how much we aggravate the injury. Some people won’t stop working for 3 or 4 days to let things start healing.
[…]
In 1978, in my 2nd quarter of chiropractic school, I blew a disc while
deadlifting in a competition. It took me 8 weeks to recover. No surgery.
Just chiropractic. I came back just as strong and the following year I set
personal and state records, etc. at 123. So I know first hand about back
injuries. I’ve had my share of them. That’s one of the reasons I stayed out
of it for so long.
Vince’s mail is a good foundation for reflection on the inherent injury risk in powerlifting. There is no denying that powerlifting is a high-risk activity and injuries do happen. Some would go as far as saying that they are part and parcel of the sport, with some critics readily proclaiming that “powerlifting will only destroy your body for life”. After spending nearly a year reading various powerlifting message boards and articles, my impression is that people come back from the overwhelming majority of injuries and become stronger than ever provided they take their rehabilitation seriously. As Vince indicates, the body knows how to heal itself as long as you give it what it needs. At the extreme end, even the most dreaded disc problems, as evidenced by Stuart McGill’s must-have work in the field Low Back Disorders, can be totally healed if treated correctly (this usually does not imply surgery). Luckily, most powerlifting injuries tend to be much more benign than this, often the result of not giving enough attention to the wear and tear that comes with heavy lifting.
The challenge of powerlifting is to learn to deal with the injury risk and accept it without fearing it. The fact of the matter is that you are not very likely to cripple yourself powerlifting, but you can reasonably expect to at least get some joint ache and possibly strain a muscle or two. It does not have to get much worse than this if you become a total technique freak (videotaping helps), listen to your body (don’t do the next set if you have a gut feeling you shouldn’t) and give your minor aches time to heal before they turn chronic. Making a point of doing heavy lifts in the safety of a power rack is also not a bad idea. Turning the issue upside down, powerlifting is liable to teach you a lot about your own body and its limitations if you can stay humble and retain some semblance of a beginner’s mind. In the final analysis, I think this is actually the real challenge of powerlifting. It is too easy to be impatient, it is too easy to go too heavy too soon lured by the prospect of a new personal record, it is too easy to blindly follow the advice of others without thinking about how it suits oneself, it is too easy to… I know, I tend to do it too, but I do try to inject the occasional dose of sense and sensibility into my training. Quoting Vince, injuries due help make the point, but it’s really not the route I’d like to go to make my points.
March 27, 2004
Trigger happy bone cruncher
Went to see the osteopath as planned on Thursday for my lower back pain, my first visit to a joint mobility specialist. After stripping down to my underwear, he had me bend forward and sideways to assess mobility. Then he poked his way down my spine and concluded that I had come just in time. “Seems like we have quite a mess here”. Just what I wanted to hear. I knew I was in good hands.
He told me to get on the bench sideways with my stomach facing him and the upper leg bent. “Now fill your lungs… exhale…”. I felt a nice crunch in my lower back as he pressed his bodyweight down on my leg. “Ok, that jumped into place. Now turn around”. Within minutes he had crunched both my lower and upper back from several angles and I was feeling increasingly satisfied with having come. He told me that my lower back was not as static as he had first thought, but I had had a lock in my upper back that must have been there for quite some time. After locating some sore points in my gluteus, he gave me a brisk but hard glute and hamstring massage. “Done!”.
Standing up, I could indeed feel the difference. My shoulders felt light and I had more ease of movement in the upper back. My lower back pain had also sharply diminished. Pointing down at my lower back, he said that three of the vertebra had been out of sync restricting full movement. “You have tight gluteus” he continued, “those often cause pain to radiate to the lower back”.
At this point I was all smiles, and blurted out that I would continue taking it careful with my lower body training and work on technique. “Nah, just don’t do any twisting movements for the rest of the day”. He then assured me that my musculature was in quite good shape and that I could begin to train hard very soon. Happily paid the 35 euro and scheduled a check-up appointment for two weeks later.
The next day, the pain had reappeared, this time to the right side. Some very light soreness was also to be felt around the spine where the therapist had exerted his well-channeled therapeutic spinal violence. Deadlift day? No way, José! Went swimming instead, figuring that it would be an ideal low strain activity with which to push some needed blood into the area. Hitting the sack in the evening I did indeed feel better.
Waking up today, I still had some light stiffness on the right side. Halfway through a morning stroll with Sanna, it stiffened up some more. Once home, Sanna pulled out The Trigger Point Therapy Workbook to see whether there could be any of those nasty buggers involved, something that looked somewhat likely as the osteopath had already suggested that the back pain could be traceable not to the back itself but to the gluteus. For those of you unfamiliar with trigger points, here’s the general enlightening gist summarized from a chapter aptly titled “All about Trigger points”:
Travell and Simons define a trigger point as “a highly irritable localized spot of exquisite tenderness in a nodule in a palpable taut band of muscle tissue”. The first part of that definition just means that a trigger point hurts like the devil when you push on it. [..] The “nodule” in the formal definition is the trigger point itself. To your fingertips, it feels like a knot or a small lump that can range in size from a pinhead to a pea. [..] The “palpable taut band” is a semihard strand of muscle that feels like a cord or cable and is easily mistaken for a tendon. Taut means it’s tightly stretched. Palpable means you can feel it with your fingers. [..]
A trigger point is not the same thing as a muscle spasm. A spasm involves a violent contraction of the entire muscle. A trigger point is a contraction in only a small part. [..]
The defining feature of a trigger point is referred pain. [..] Back pain always has a myofascial component, no matter the official diagnosis. Although arthritis, bad disks, and displaced vertebrae come quickly to mind when your back hurts, back pain very often is nothing but referred pain from myofascial trigger points. Pain in your lower back can come from trigger points in surprising places, such as your buttocks, your stomach muscles, or even knotted-up muscles in your calves. [..] Some of the activities that create trigger points are obvious, like accidents, falls, strains and overwork. [..]
Most systems of therapeutic touch, like acupressure, shiatsu, craniosacral therapy, myofascial release, Swedish massage, and even deep tissue bodywork - despite their good uses - are also too nonspecific to guarantee success with trigger points. For dependable results, therapy needs to be applied directly to the trigger point. [..] The safest and most effective method of trigger point therapy, according to Travell and Simons, is deep stroking massage applied directly to the trigger point.
Davies, Clair (2001): The Trigger Point Therapy Workbook. New Harbinger Publications; pp. 17-33.
 I have briefly mentioned trigger points before in the shoulder context. For much of September I had problems with my right shoulder which would get very tender after benching. Unlike other trigger points, those in the shoulder do often not refer pain, so in this case locating the source of the trouble was easy enough. It cleared up with some hard direct massage of the trouble spot. In December and January, the problem returned. Although I did not write about it in the blog, I had some fears that I might not be able to complete the benching intense Prilepin bench program if it turned out that the shoulder could not take it. After Sanna bought the above book, I learned that these problems are very easy to take care of oneself with the aid of a tennis ball, or similar, which is placed between the wall and the trigger point. Massaging the trigger point hard (pain should be roughly 7-8 on a scale from 1 to 10) in one direction for one minute several times a day once or twice a week results in instant relief and keeps shoulder pain away completely. The chance of the back problem being in the same league sounded almost too good to be true.
I have briefly mentioned trigger points before in the shoulder context. For much of September I had problems with my right shoulder which would get very tender after benching. Unlike other trigger points, those in the shoulder do often not refer pain, so in this case locating the source of the trouble was easy enough. It cleared up with some hard direct massage of the trouble spot. In December and January, the problem returned. Although I did not write about it in the blog, I had some fears that I might not be able to complete the benching intense Prilepin bench program if it turned out that the shoulder could not take it. After Sanna bought the above book, I learned that these problems are very easy to take care of oneself with the aid of a tennis ball, or similar, which is placed between the wall and the trigger point. Massaging the trigger point hard (pain should be roughly 7-8 on a scale from 1 to 10) in one direction for one minute several times a day once or twice a week results in instant relief and keeps shoulder pain away completely. The chance of the back problem being in the same league sounded almost too good to be true.
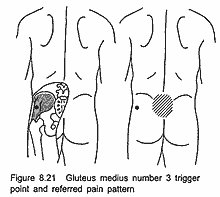
Sanna got me on her massage bench and started feeling her way through my gluteus, hamstrings and calves. The end result was that she located one tender spot on both gluteus (the left one is probably the one shown in the picture), plus one on the right calf muscle. Although it is not very easy to determine whether the gluteus ones are indeed true trigger points, or just local stiffness, due to the heavy layer of fat and muscle on top (I like to think more of the latter), initial treatment of these spots with a tennis ball against the wall have shown positive results. Invariably, most of the pain has dissipated for some time, save for the local gluteus tenderness caused by the ball. Based on her experience with clients, Sanna told me that the gluteus tend to get sore very easily from hard massage. I am taking it a little easier now with the ball to allow some of the soreness to disappear, but do hit them hard a few times per day. I will continue doing this for a while. I gather it is the only way to find out if this removes the back stiffness or not. I have also started massaging the shoulder trigger points several times a day in an effort to totally get rid of them instead of just pacifying them for the moment.
But where did this back trouble come from? From the type of pain, I can tell that this is not the ligament sprain reappearing. Besides, much of this stiffness has been off to the sides, not at the old injury spot in the middle of the lower back. The scenario that appears most likely is that this new back pain is a direct by-product of other muscles having had to protect the back injury and trying to compensate for the loss of back strength. Hence the displaced vertebrae and the tight gluteus; they could not cope with this increased burden and imbalanced musculature. In this context trigger points could also very easily develop if we are to trust Davies’s argument. In fact, he states that trigger points are often latent at first (they can be for years or forever), but then suddenly become active when straining (such as performing a heavy lift or getting into an awkward position). This would be a plausible explanation for why I suddenly started feeling pain on the left side of my lower back when squatting on Monday.
Trigger points or not, we will just have to see how things develop from here. In the meantime, I highly recommend buying the trigger point book. The fact that Dave Tate’s Elite Fitness Systems also stocks this book should testify to its importance for powerlifters. You might be pleasantly surprised to find out that you can clear up your pain with just a tennis ball.
March 22, 2004
One of those days
Second go at squats powerlifting style without a box. Thought I would go for 3x3 with something like 75 kg/166 lbs or 80 kg/177 lbs. Everything went so-so until I did 3 @ 70 kg/155 lbs, when the left side of my hip towards the back decided to stiffen up on the second rep. I’ve had things like this before; hopefully it will go away with some rest and massage. How smart is it to continue doing a third rep after feeling that something is not quite right on the second rep? Plain stupid. I’ve never been one to stop a set as long as I’m not injured, but it is high time I learn this noble art. And how smart is it doing good mornings following this? “The pain is to the side, will probably feel better after some light GMs”… Plain very darn stupid, that’s what. The fact that I stopped here without continuing with calves and abs gives a glimmer of hope for the future.
Did tape my squats and tried hard to get the elbows in instead of flaring them back. Overall, today’s clips do not really represent any improvement over those from ten days ago, if anything these sets look worse (you will just have to trust me on this, ain’t gonna upload ‘em). Simply wasn’t my kind of training day today. Give it a rant on the blog and move on. Preferably into a nice pre-warmed bed. ![]()
Squat:
3 @ 40 kg/88 lbs
3 @ 50 kg/111 lbs
3 @ 60 kg/133 lbs
3 @ 70 kg/155 lbs
Good morning, depth at 6 pin:
10 @ 30 kg/66 lbs
10 @ 40 kg/88 lbs
10 @ 50 kg/111 lbs
Total training time: something like 25 minutes or so
January 30, 2004
First contact
 With the Zercher commandos having done good reconnaissance along the Ripped Back frontier, it was time to up the ante and bring in the 13″ box squat. The perimeter being far from secured, I staid a safe sounding 15 kg/33 lbs below my max from the pre-injury days of November. That being said, the last single with 100 kg/221 lbs felt heavy enough after not having maxed out on these for a few months.
With the Zercher commandos having done good reconnaissance along the Ripped Back frontier, it was time to up the ante and bring in the 13″ box squat. The perimeter being far from secured, I staid a safe sounding 15 kg/33 lbs below my max from the pre-injury days of November. That being said, the last single with 100 kg/221 lbs felt heavy enough after not having maxed out on these for a few months.
Tapping the back with a heavier stick was not my only objective today. Pushing the torso forward and the head back was a supremely good reason to get in under the bar after those fairly nasty looking Zerchers. I am happy to report that these looked better (video 3.8M), although things degenerated a little towards the end. It was suggested over at westsidebar.net that the tendency to good morning the weight up might actually be indicative of a strong back and weak legs; first do the easy part (extend the legs), then finish it off with a good morning. I have always wondered what the point of bending the legs in the deadlift is…
One flaw that quite literarily sticks out in the video is the elbows. Next time I vow to keep them aligned under the bar. As Tate writes:
When your elbows turn out toward the back, the bar will drift forward again and end up stapling you to the floor as well as ripping your head off. This is one common mistake I see in all my seminars.
My shins seem to be fairly vertical, but I could definitively sit back a little further. I also need to look into spreading the knees and pushing the feet out. Work to be done, work to be done…
Box squat, 13″:
5 @ 50 kg/111 lbs
1 @ 60 kg/133 lbs
1 @ 70 kg/155 lbs
1 @ 80 kg/177 lbs
1 @ 90 kg/199 lbs
1 @ 100 kg/221 lbs
Pull-through, bent legged: 3x12 @ 90 kg/199 lbs
Standing cable crunch, lat pulley: 3x10 @ 40 kg/88 lbs
Total training time: 48 min
January 19, 2004
More bright ideas
It’s been a while since I did one of those zombie workouts after little or no sleep. Today was such a day. Began my spring term teaching at the University of Helsinki today with a course in English on Tibetan history. As usual making pdfs of supplementary readings, maps etc. demanded the whole night save for one tiny hour of sleep between 10am and 11am. No wonder then that speed benching went so-so, and I had real trouble getting my upper back pushed into the bench on rack lockouts.
Somehow I got the bright idea to do cable rows with sub-max weights to see how the you-know-what would handle it. It is hard to describe how it felt, but I could tell my lower back was not quite ready for these yet. Movements which allow me to maintain a back arch work quite well now, but these round back thingies are still out of the question (I like to streeeetch on these).
First go at the delt supersets. Did front raises, side raises and power cleans back to back sitting on the edge of a bench, which worked well except that I could not muster any clean reps on the cleans (uncleans?). Next time I’ll switch the order around which should work better (weakest muscles first, strongest last).
Before black-out I still need to write my lecture for the Chinese intermediate course I’m teaching every Tuesday. Pretty ok schedule compared to last spring term when I lectured three days in a row. Oh yes, almost forgot. Just placed a pick-up order on a digital camera (Canon Powershot A80); perhaps I will do some Zercher squats on Wednesday and tape them. Until then, train hard!
Speed bench; narrow, medium, wide: 9x3 @ 60 kg/133 lbs
Close-grip Rack lockouts, 4th pin:
5 @ 50 kg/111 lbs
3 @ 70 kg/155 lbs
1 @ 80 kg/177 lbs
1 @ 90 kg/199 lbs
0 @ 102.5 kg/227 lbs
0 @ 100 kg/221 lbs (dropping like this never works, so why did I do it?)
Seated cable rows, close-grip: 2x5 @ 90 kg/199 lbs
2 supersets:
Seated front raise: 2x6 @ 12 kg/27 lbs
Seated side raise: 2x6 @ 12 kg/27 lbs
Seated dumbell power clean: 4 @ 12 kg/27 lbs, 3 @ 10 kg/22 lbs
Total training time: 26 min